ORBITA-AF
Feasibility study of an objective randomized blinded investigation of therapeutic ablation versus cardioversion for persistent Atrial Fibrillation (ORBITA-AF).
Full Title: Feasibility study of an objective randomized blinded investigation of therapeutic ablation versus cardioversion for persistent Atrial Fibrillation
Short Title: ORBITA-AF
Sponsor: Barts Health NHS Trust
Funder: Barts Charity, MEDTRONIC
Chief Investigator: Professor Richard Schilling
Co-Investigators: Dr Malcolm Finlay, Principal Investigator, Barts Health NHS Trust
Contact: malcolm.finlay1@nhs.net
Study Design: Feasibility randomised, blinded, controlled trial
Objectives:
- To assess the feasibility of an objective, randomised, blinded investigation comparing catheter ablation and cardioversion for persistent atrial fibrillation
- To evaluate procedures for recruitment, data collection and monitoring using long-term implantable cardiac monitors
Number of Participants: 20
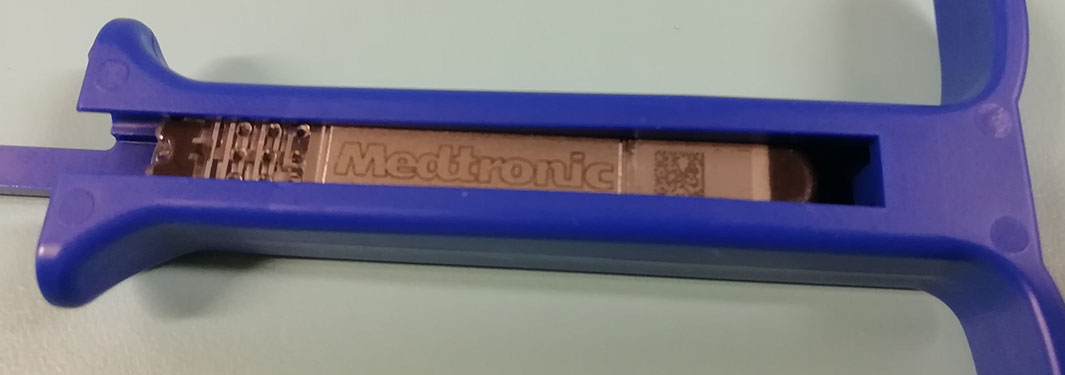
Devices Used: Implantable cardiac monitors (miniaturised, long-term injectable)
Study Duration: 6 months
Location: Barts Health NHS Trust
Summary: This feasibility study aimed to determine the best treatment approach for patients with persistent atrial fibrillation (AF) who are candidates for rhythm control therapies. Currently, many such patients are offered an electric shock procedure called cardioversion to restore normal heart rhythm. However, this intervention often fails to provide lasting results, with many patients requiring ongoing medication to maintain a normal rhythm.
Catheter ablation is a more recent intervention shown in several studies to have better outcomes in maintaining sinus rhythm than cardioversion. However, no trials have directly compared these treatments in a blinded, randomised design for this patient population.
In this study, eligible patients were implanted with a miniaturised, long-term injectable cardiac monitor to allow continuous monitoring of heart rate and rhythm. Participants were then randomised to receive either cardioversion alone or cardioversion combined with catheter ablation. After hospital discharge, they were followed up in outpatient clinics with regular rhythm assessments. The study’s outcomes will inform the design of a future definitive trial.

